Why It Matters
Understanding the role of the Payer Connector is crucial for health IT leaders seeking to reduce manual data handling and improve interoperability between Epic and payer ecosystems. As payers grapple with siloed architectures, effective integration can accelerate value‑based care initiatives and position organizations to leverage emerging AI tools for better decision‑making.
The Fight for Payer Control Points
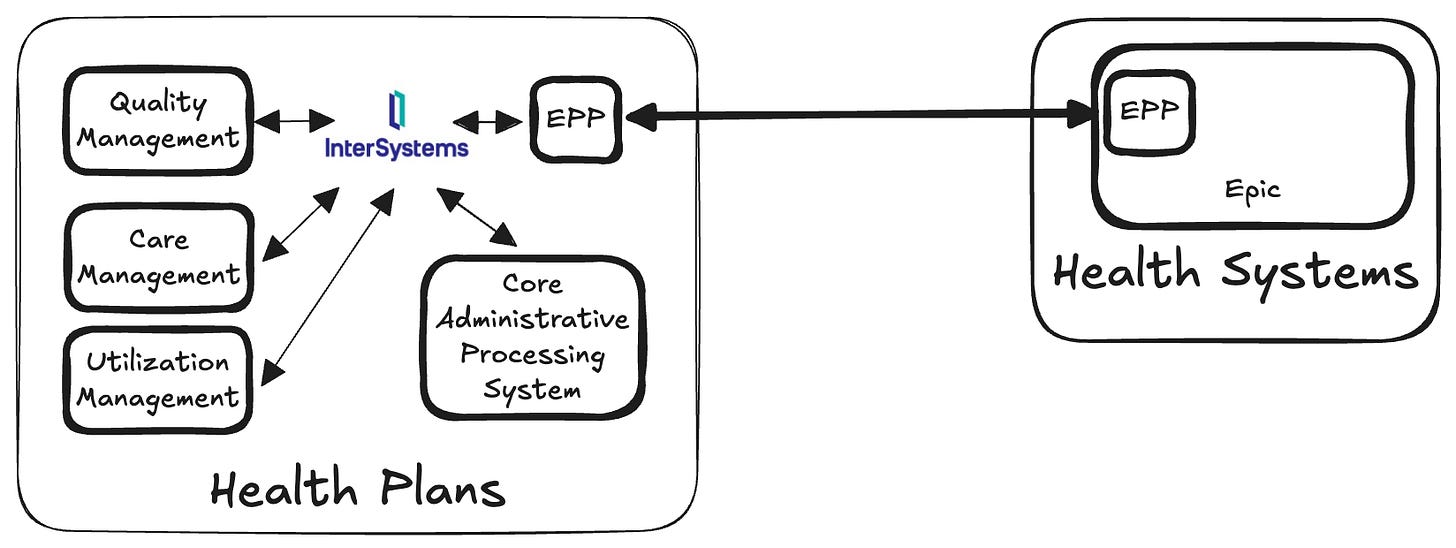
InterSystems announced a noteworthy product launch, their Payer Connector, on the Epic Showroom. A few conversations afterward suggested people were misreading what it actually is, so it’s worth being direct about where it fits in the interoperability stack.
[
](https://substackcdn.com/image/fetch/$s_!BkHY!,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4969f6da-7731-492a-ad71-0186dc42cac8_1648x620.png)
Straight to the point - this is not a competitor to Epic Payer Platform. It is a complementary product, sold to payers, designed to help them operationalize Epic Payer Platform by connecting it to the rest of the payer’s internal environment.
Think of Epic Payer Platform as the payer-facing edge of Epic: a standardized, opinionated interface into Epic health systems. InterSystems’ Payer Connector sits behind that edge":
Targeted routing delivers needed data to claims, care management, UM, quality, analytics, and member systems – and sends back those insights, reducing manual intake and overhead.
Provider and payer IT landscapes are at very different points on the consolidation curve. Health systems have spent the last decade moving from best-of-breed applications toward a single enterprise operating system. Payers largely have not. Their internal boundaries of lines of business, delegated entities, product teams, and analytics groups are often rigid, deeply entrenched, and governed like semi-autonomous domains.
A single, unified system that cuts cleanly across those boundaries is thus politically threatening. That social barrier challenges ownership, budget control, and decision rights. In this era of outsized advantage (via LLMs) towards shared knowledge and context, we’ll see innovative organizations push towards more unified systems.
However, that is some time off. InterSystems’ offering plays to their strength as an Integration Platform as a Service. There are other players here, like Rhapsody or Mergence Health. This is just a formalization and marketing of their strengths to a newer (and undoubtedly growing) market segment.
The Bigger Picture
Where things get more interesting (at least for me) is mapping this to a few other things that have happened in the past weeks related to Epic and payers.
First, Epic has done a trajectory U-turn and full Michael-Jordan-memed in regards to Epic Payer Platform:
[

](https://substackcdn.com/image/fetch/$s_!0B5p!,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2Fb5bb8911-d30f-4737-a906-5affb026eb2d_800x500.jpeg)
The drought is certainly over. Since UPMC was announced, we have seen two additional payers sign on:
0
Comments
Want to join the conversation?
Loading comments...