Diabetes Is Linked to Higher Risk of Pancreatic Cystic Neoplasms
•February 13, 2026
0
Companies Mentioned
Why It Matters
The link between chronic diabetes and PCNs signals a potential need to refine surveillance guidelines, balancing early detection with cost‑effective care for a prevalent population.
Key Takeaways
- •Diabetes raises PCN risk up to 37%
- •Risk escalates with diabetes duration
- •Younger men and smokers face higher PCN odds
- •Only 4.1% of PCNs progressed to cancer
- •Study based on Korean NHIS data
Pulse Analysis
The new Korean cohort analysis adds a crucial epidemiologic layer to the growing conversation about metabolic disease and pancreatic health. By leveraging the Korean National Health Insurance Service, researchers tracked over 3.8 million adults for a decade, revealing a clear gradient: longer diabetes exposure translates into higher pancreatic cystic neoplasm incidence. This dose‑response relationship aligns with prior observations that hyperglycemia and insulin resistance may foster a pro‑tumorigenic microenvironment, yet the sheer scale of the dataset lends unprecedented statistical power to the association.
Clinicians interpreting these findings must balance vigilance with practicality. While the data suggest that diabetes—especially beyond five years—elevates PCN risk, the absolute incidence remains low (0.82 per 1,000 person‑years). Consequently, universal imaging of asymptomatic diabetic patients would likely generate excessive downstream procedures without proportional benefit. Instead, the study supports a risk‑stratified approach: consider pancreatic imaging when cysts are incidentally discovered, when patients present additional risk factors such as smoking, or when clinical symptoms arise. This nuanced stance helps avoid over‑diagnosis while ensuring high‑risk individuals receive appropriate attention.
Looking ahead, the research highlights gaps that future investigations should address. The reliance on ICD‑10 codes precludes differentiation among cyst subtypes, which vary markedly in malignant potential. Moreover, the homogeneous East Asian cohort raises questions about generalizability to Western populations with differing genetic and lifestyle profiles. Integrating imaging data, medication histories, and biomarkers could refine risk models and guide personalized surveillance protocols, ultimately improving outcomes for patients navigating the intersection of diabetes and pancreatic disease.
Diabetes Is Linked to Higher Risk of Pancreatic Cystic Neoplasms
Pearl Steinzor · Fact‑checked by: Giuliana Grossi · February 13 2026
Diabetes was associated with an increased risk of pancreatic cystic neoplasms (PCNs), with longer disease duration linked to progressively higher risk, according to a nationwide population‑based cohort study of more than 3.8 million adults in Korea published in JAMA Network Open [1].
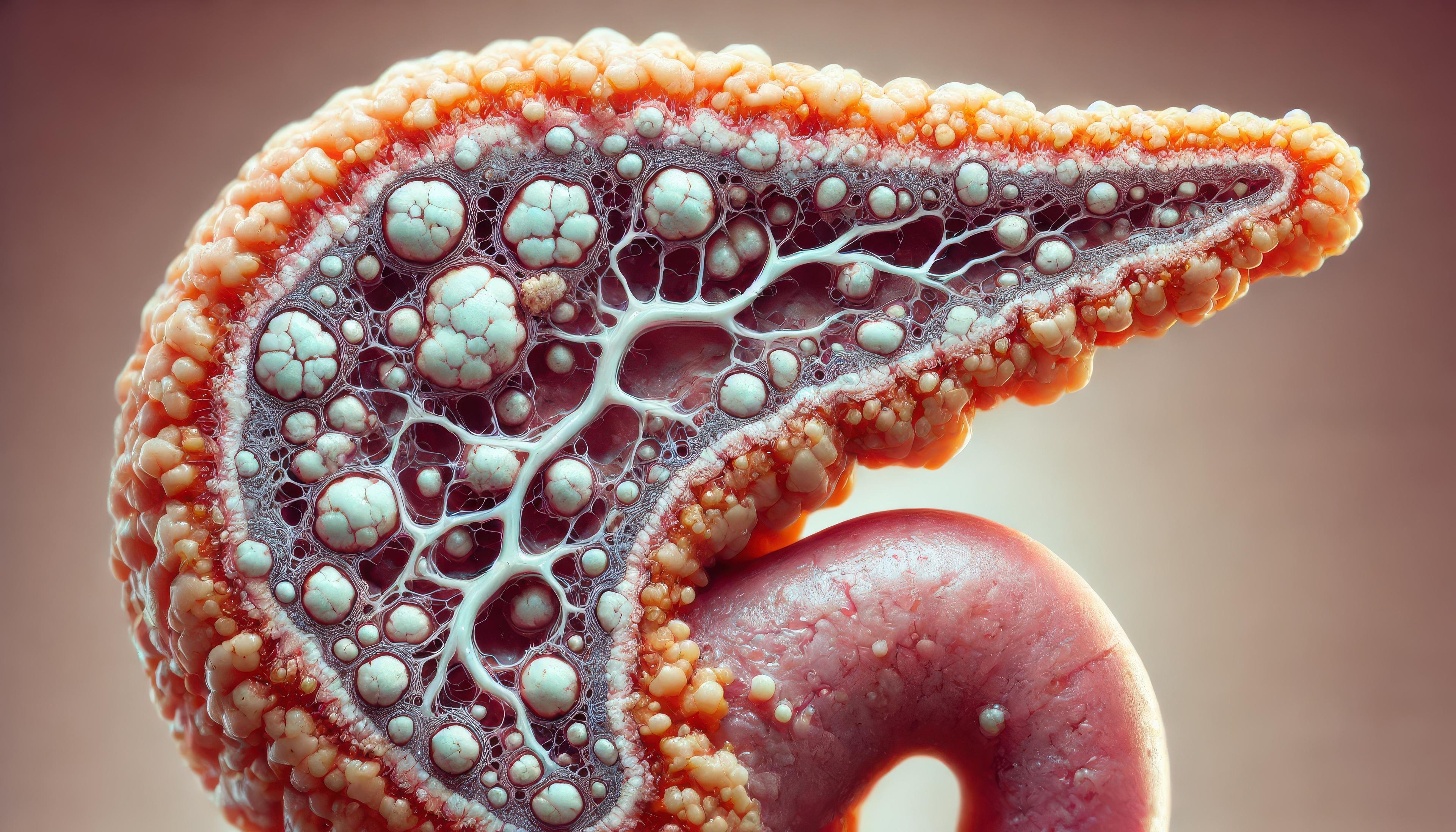
![Pancreatic disease in diabetes]
Longer diabetes duration was associated with a significantly increased risk of pancreatic cystic neoplasms. | Image credit: Ross – stock.adobe.com
“These findings underscore the need for cautious interpretation: while the presence of a cyst may signal an elevated malignant potential in some cases, population‑wide surveillance of all cystic lesions, particularly among patients with diabetes (a highly prevalent condition), may not be justified,” wrote the researchers of the study.
The cohort study used data from the Korean National Health Insurance Service (NHIS), which covers approximately 97 % of the Korean population. Adults aged 20 years or older who underwent a standardized health examination in 2009 were eligible. After exclusions for missing data, prior pancreatic cysts, pancreatitis‑related conditions, or diagnoses within a 1‑year lag period, 3,856,676 individuals were included and followed through December 31, 2020. Data were analyzed from March 23 2023 to February 8 2024.
Participants were categorized by glycemic status as:
-
Normoglycemic (fasting glucose < 100 mg/dL)
-
Impaired fasting glucose (100–125 mg/dL)
-
Diabetes < 5 years duration
-
Diabetes ≥ 5 years duration
Diabetes was defined using ICD‑10 codes, antidiabetic medication prescriptions, and fasting glucose levels. Incident pancreatic cysts were identified using ICD‑10 codes K86.2, D13.6, and D37.7, with exclusions to minimize inclusion of non‑neoplastic cysts.
Adjusted hazard ratios (AHRs) for PCN occurrence were estimated using Cox proportional hazards models.
Model 1 adjusted for age, sex, hypertension, dyslipidemia, income, smoking status, alcohol consumption, regular physical activity, and body‑mass index;
Model 2 additionally adjusted for hypertriglyceridemia.
Key Findings
-
Among 3,856,676 adults (mean [SD] age 47.1 [14.0] years; 54.5 % male), 330,138 (8.6 %) had diabetes.
-
Median follow‑up was 10.3 years (IQR 10.1‑10.6), totaling 38,906,756.3 person‑years.
-
During follow‑up, 31,877 individuals (0.8 %) developed PCNs (incidence 0.82 per 1,000 person‑years).
Incidence rates by glycemic category
| Category | Incidence (per 1,000 person‑years) |
|----------|------------------------------------|
| Normoglycemia | 0.72 (95 % CI 0.71‑0.73) |
| Impaired fasting glucose | 0.89 (95 % CI 0.87‑0.91) |
| Diabetes < 5 years | 1.25 (95 % CI 1.20‑1.30) |
| Diabetes ≥ 5 years | 1.82 (95 % CI 1.74‑1.90) |
Multivariable‑adjusted AHRs (vs. normoglycemia)
-
Impaired fasting glucose: 1.06 (95 % CI 1.03‑1.08)
-
Diabetes < 5 years: 1.23 (95 % CI 1.18‑1.28)
-
Diabetes ≥ 5 years: 1.37 (95 % CI 1.31‑1.44)
Subgroup analyses
-
Age < 60 years: AHR 1.34 (95 % CI 1.27‑1.40) vs. age ≥ 60 years: AHR 1.21 (95 % CI 1.16‑1.27) (P = .003)
-
Men: AHR 1.32 (95 % CI 1.26‑1.38) vs. women: AHR 1.20 (95 % CI 1.15‑1.26) (P = .005)
-
Current smokers with diabetes: AHR 1.40 (95 % CI 1.30‑1.51) vs. never‑smokers 1.22 (95 % CI 1.18‑1.28) and former smokers 1.25 (95 % CI 1.16‑1.35) (P = .006)
-
Of the 31,877 individuals with PCNs, 1,315 (4.1 %) were subsequently diagnosed with pancreatic cancer.
-
Overall, 25,517 participants (0.7 %) developed pancreatic cancer during follow‑up.
Limitations
-
PCNs were identified using administrative ICD‑10 codes; imaging data were unavailable.
-
Residual confounding cannot be excluded despite multivariable adjustment.
-
Observational design precludes causal inference.
An accompanying editorial highlighted methodological constraints, including reliance on ICD‑10 codes that do not distinguish cyst subtypes, lack of imaging granularity, limited data on antidiabetic therapies, and the homogeneous East Asian cohort, which may affect generalizability [2].
“Cho et al. provide valuable epidemiologic evidence that diabetes—particularly long‑standing diabetes—is associated with an increased likelihood of a newly diagnosed pancreatic cyst,” wrote the authors. “For clinicians, the message is one of contextualized vigilance: diabetes should not trigger pancreatic imaging in the absence of symptoms or other risk factors, but it may inform diagnostic interpretation once a cyst is identified.”
Conclusion
Diabetes, especially when present for ≥ 5 years, is associated with a progressively higher risk of pancreatic cystic neoplasms. Risk rises with worsening glycemic status and is more pronounced in younger individuals, men, and current smokers. These findings suggest that diabetes status and modifiable lifestyle factors may influence PCN development and could inform future surveillance strategies.
References
-
Cho IR, Chang SH, Lee SH, et al. Pancreatic cystic neoplasm risk among individuals with diabetes. JAMA Netw Open. 2026;9(2):e2556951. doi:10.1001/jamanetworkopen.2025.56951
-
Crippa S, Piemonti L. Diabetes and pancreatic cystic neoplasms—dangerous liaisons. JAMA Netw Open. 2026;9(2):e2556869. doi:10.1001/jamanetworkopen.2025.56869
0
Comments
Want to join the conversation?
Loading comments...