New Method Can Find Hidden Eggs to Aid in Fertility Treatment
•February 12, 2026
0
Why It Matters
Increasing egg recovery directly raises the odds of viable embryos, potentially shortening treatment cycles and lowering costs for patients and clinics.
Key Takeaways
- •Device added eggs for 54% of patients
- •Recovered 582 extra eggs from 582 patients
- •One extra egg produced a successful live birth
- •Automation may alleviate embryologist shortages
- •FDA clearance required before clinical adoption
Pulse Analysis
The bottleneck in in‑vitro fertilization often lies not in fertilization itself but in the initial egg‑retrieval step. Conventional embryologists manually examine follicular fluid under high‑powered microscopes, a labor‑intensive process that discards a substantial portion of the sample. OvaReady leverages microfluidic channels and pinball‑like bumpers to sift fluid automatically, exposing eggs that would otherwise be lost. By converting a previously wasteful by‑product into a source of viable oocytes, the device addresses a long‑standing inefficiency in reproductive medicine.
The Nature Medicine study demonstrated that OvaReady identified extra eggs in more than half of the 582 patients examined, adding 582 previously uncounted oocytes to the pool. This increase translates into a higher probability of generating quality embryos, as evidenced by the successful pregnancy and birth reported in the trial. For clinics, the automation promises to standardize a critical step, reduce technician fatigue, and free skilled embryologists to focus on embryo culture and genetic screening. In regions where reproductive specialists are scarce, such technology could level the playing field, offering patients comparable outcomes without the need for extensive manual expertise.
Regulatory clearance remains the next hurdle. While AutoIVF is engaging the FDA, the device is currently available only within research protocols. Should approval be granted, the market could see rapid adoption, especially as IVF cycles increasingly rely on intracytoplasmic sperm injection, a workflow already compatible with OvaReady’s denudation feature. Future iterations may expand to conventional IVF, further broadening its utility. Continued large‑scale trials will be essential to confirm that the additional eggs consistently produce high‑grade embryos and live births, cementing the technology’s role in the next generation of fertility treatments.
New Method Can Find Hidden Eggs to Aid in Fertility Treatment
Feb. 12, 2026
Pam Belluck is a health and science reporter for The Times, covering a range of subjects, including reproductive health, long Covid, brain science, neurological disorders, mental health and genetics.
Fertility experts know that the more eggs retrieved from a woman, the better the chances that one of them will lead to a viable embryo that will result in the birth of a baby.
Now, a new study suggests something startling, even to many in the field: the conventional method of searching for eggs often fails to find all of them, and a new technology that automates the process may significantly increase the number recovered.
Using the conventional method, embryologists use high‑powered microscopes to search the follicular fluid extracted from women in fertility clinics. The fluid is then discarded. The study, published in Nature Medicine on Thursday, reported that a device that uses microfluidic technology to sift through follicular fluid found additional eggs for more than half of the patients.
“It’s very, very surprising,” said Dr. Mitchell Rosen, who directs the reproductive laboratories at the University of California, San Francisco and was not involved in the study. “They were finding eggs that we wouldn’t otherwise have had the potential to use.”
The device runs the fluid through a series of pinball‑machine‑like bumpers and lanes. In the study, it searched about‑to‑be‑discarded fluid from 582 patients in four clinics that had already been examined by hand using microscopes. The device recovered extra eggs in the fluid from 316 of the patients, finding a total of 582 additional eggs.
In another part of the study, involving 19 patients, an embryo formed from an egg recovered by the device led to a successful pregnancy for a couple, whose daughter was born in September.

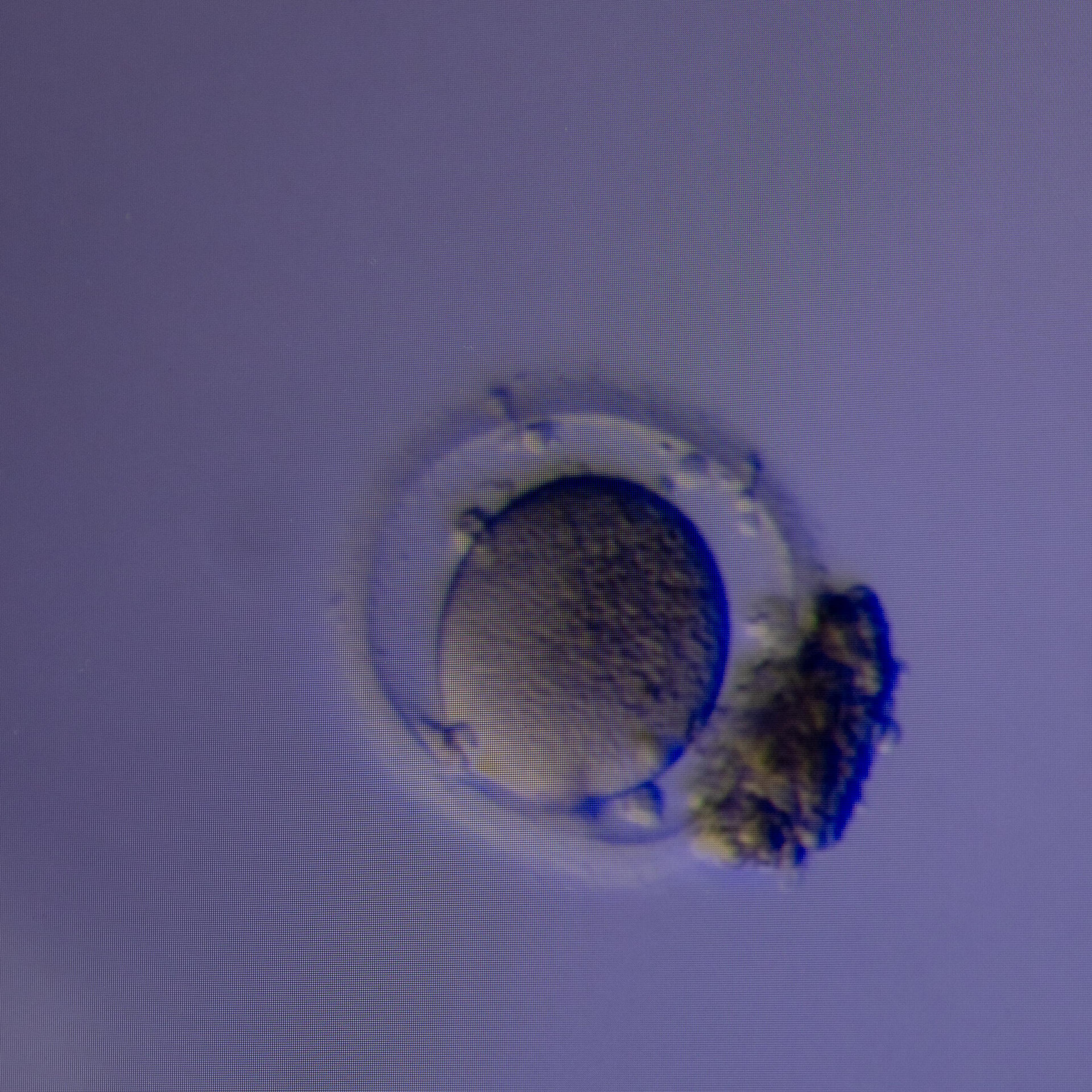
The new technology may significantly increase the number of eggs recovered from patients. Credit…Cassandra Klos for The New York Times
In an interview, the couple—who asked that their names be withheld to protect their privacy—said they had tried to conceive naturally for 18 months and then undergone a fertility‑treatment cycle that did not result in embryos.
“We just lost all hope and had to start grasping at straws,” said the father, 35. When the clinic asked if they wanted to participate in the study of the new device, he said they immediately agreed.
“It found eggs that otherwise would have been discarded,” the mother, 33, added, noting that their baby was healthy.
The study was conducted by the company that developed the technology, AutoIVF of Natick, Mass., and supported by a grant from the National Institute of Child Health and Human Development, part of the National Institutes of Health.
Ravi Kapur, chief executive officer of AutoIVF and an author of the study, said the device, called OvaReady, was originally intended to increase efficiency and standardization of a key step in the fertility process: finding and isolating eggs so they can be fertilized by sperm. In recent years, other technology advances have automated other fertility steps.
Dr. Kapur said his team had thought the device might find “some eggs being left behind,” perhaps in 10 percent of cases, but “not the 50 percent consistently across multiple very high‑end clinics in this country.” (He noted that the four clinics in the study, one of which provided most of the samples, were in the eastern United States and part of larger networks, but confidentiality agreements prevented him from identifying them.)
He said AutoIVF is in discussions with the Food and Drug Administration and will seek approval to use the device in clinical practice. In the meantime, clinics can offer it as part of research efforts.
Dr. Kapur said he expected some clinics to process a patient’s “entire follicular fluid” using the device, while others “might take a little bit more of a conservative approach,” running half of a patient’s sample through OvaReady and examining the other half conventionally before checking it with the device. The company has yet to determine a price for the device.
Fertility experts not involved in the research said larger studies were needed to confirm the results, and especially to indicate how often eggs found by the device could produce high‑grade embryos, and how often those embryos could lead to live births.
“These are promising findings,” said Dr. Elnur Babayev, an assistant professor at Northwestern University specializing in reproductive endocrinology and infertility, who was not involved in the study but reviewed it for the journal before publication.
Key questions remain, he said: “Is that going to increase the likelihood that any given patient will have a baby using that technology, and how many babies will they have?”
Rebecca Robker, a professor of reproductive biology at Adelaide University in Australia, cautioned that the study involved only a small number of patients whose eggs were fertilized into embryos, and one birth, so it does not prove the technology will lead to more babies. However, she noted, “they showed that these extra eggs weren’t small, shriveled‑up eggs that they didn’t want anyway. These were viable eggs that were being found.”

A part of the OvaReady system, used to isolate and denude eggs. Credit…Cassandra Klos for The New York Times
Still, Dr. Robker said, “in my view, it should be used as a backup and as a safety check,” not replacing the conventional method, but “verifying that every egg has been found.”
Some experts said the technology might eventually become the primary method for searching follicular fluid, helping embryologists focus more on other responsibilities—especially in less populated areas where embryologists are in short supply.
Experts noted that in the study the device was used only with a method in which sperm is injected into eggs, called intracytoplasmic sperm injection (ICSI), not conventional IVF, because OvaReady conducts a step called denudation, removing cells around an egg in preparation for ICSI. Dr. Kapur said that nearly 80 percent of fertility patients use ICSI, and that another version of OvaReady could skip denudation for conventional IVF patients.
After experiments with cow eggs, the team added human eggs to fluid donated by patients after it had been searched conventionally. To the authors’ surprise, the device found extra eggs, not just those they had added.
To see if eggs found by the device could become viable embryos, the team used it to screen follicular fluid from 19 patients that had already been manually searched. For 11 of those patients, it found at least one additional egg, yielding 23 eggs the conventional search had missed. Twelve of the 23 were mature enough for fertilization. Of those, four were fertilized into early‑stage embryos (blastocysts) that were of good enough quality to be frozen for use.
By comparison, the conventional method found 225 eggs, 175 of which were mature enough for fertilization. Of those, 39 produced blastocysts that were good enough for use.
Traditionally, embryologists use high‑powered microscopes to search follicular fluid for eggs.
One of the OvaReady blastocysts was implanted in the woman who gave birth in September. The woman, who like her husband is a physician, said their first cycle at the clinic, Boston IVF, had yielded “a normal number of eggs, but it resulted in zero embryos.”
For their second cycle, Dr. Lauren Murphy, a reproductive endocrinologist at Boston IVF, asked if they wanted to participate in the study. For that cycle, Dr. Murphy also changed the type of the man’s sperm that was used, hoping to address factors that might have impeded the first cycle.
The device found four additional eggs in the woman’s follicular fluid, three of which became embryos. For reasons that are unclear, the highest‑quality embryos were among those three.
“Then the question became, are we OK with implanting the embryo that resulted from it, because they’ve never had a human live birth from these eggs,” the woman said. “We thought about it. I think the biggest question is does the device impact the egg in any way that would be harmful?”
After consulting with Dr. Murphy, they decided to transplant that embryo. The pregnancy was full‑term, without complications, and their daughter is “boisterous, she eats a ton, like a regular baby.”
0
Comments
Want to join the conversation?
Loading comments...