Leveraging AI to Predict Patient Deterioration
•February 16, 2026
0
Why It Matters
Early, AI‑driven alerts can prevent catastrophic events, improve outcomes, and close the gap between algorithm development and real‑world clinical impact.
Key Takeaways
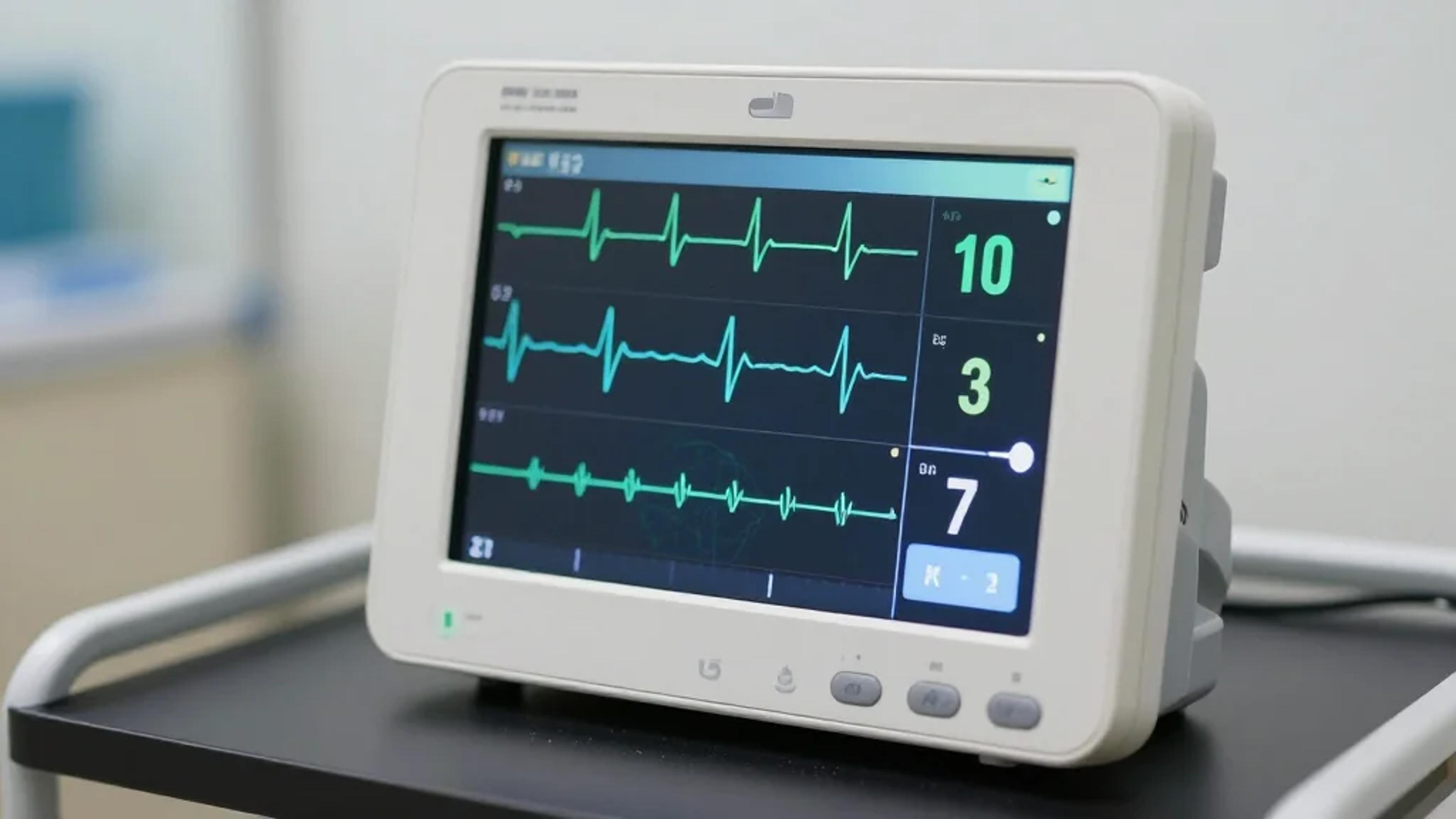
- •AI uses continuous cardiorespiratory data for early alerts
- •Real-time monitoring outperforms retrospective EHR predictions
- •Integration requires workflow-aligned score delivery
- •Scalable infrastructure needed for live data pipelines
- •Multidisciplinary strategy essential for successful clinical adoption
Pulse Analysis
The rise of artificial intelligence in acute care is shifting focus from static electronic health records to dynamic, continuous monitoring streams. By feeding cardiorespiratory waveforms into machine‑learning models, hospitals can generate predictive risk scores minutes before a patient’s condition deteriorates. This real‑time visibility transforms clinicians from reactive responders into proactive decision‑makers, potentially reducing intensive‑care admissions and mortality rates. The HIMSS26 session underscores how these predictive insights differ fundamentally from traditional retrospective analytics, offering a tangible advantage in fast‑moving environments such as emergency departments and intensive care units.
Despite the promise, many predictive models stall at the “last‑mile” of implementation. Successful translation requires more than a high‑accuracy algorithm; it demands seamless integration into existing workflows, secure and scalable data pipelines, and real‑time score delivery at the point of care. Institutions often lack a unified infrastructure that can ingest heterogeneous bedside signals, run multiple models concurrently, and distribute results securely to clinicians’ dashboards. Overcoming these technical and organizational barriers is essential to move from pilot studies to enterprise‑wide adoption, ensuring that AI recommendations are timely, trustworthy, and actionable.
For the broader health‑tech ecosystem, mastering this integration will unlock scalable, cross‑institutional deployment of predictive analytics. Multidisciplinary collaboration—uniting data scientists, clinicians, IT, and operations—creates a feedback loop that refines models and aligns them with clinical priorities. As hospitals invest in interoperable platforms and edge‑computing capabilities, AI‑driven early warning systems can become a standard component of patient safety protocols. Spaeder’s session at HIMSS26 aims to equip leaders with the roadmap needed to operationalize these technologies, ultimately driving measurable improvements in patient outcomes and setting a new benchmark for digital health innovation.
Leveraging AI to predict patient deterioration
Dr. Michael Spaeder, professor in the department of pediatrics at the University of Virginia, tells MobiHealthNews about his upcoming talk at the 2026 HIMSS Global Health Conference & Exposition in March, where he'll discuss how AI‑enabled analysis of continuous bedside monitoring data can detect patient deterioration.
MobiHealthNews: Can you give our audience a preview of what you’ll discuss during your session?
Dr. Michael Spaeder: During our HIMSS26 session, we’ll explore how continuous cardiorespiratory monitoring data can be leveraged through AI and machine learning to detect sub‑acute, potentially catastrophic health events earlier than traditional approaches. We’ll explain the difference between predictive insights from continuous monitoring versus the reflective insights from the electronic health record, highlighting why real‑time physiologic data provides a critical advantage.
We’ll also discuss best practices for deploying, integrating and evaluating these predictive analytical models in the hospital environment, including strategies to ensure clinical adoption, multidisciplinary collaboration and measurable impact on patient outcomes. Attendees will leave with a clear understanding of how to harness continuous monitoring data to improve early detection and decision‑making in acute care.
MHN: Why do so many predictive analytics models fail to translate into real‑world clinical use?
Spaeder: Although predictive models are promising, the creation of a new algorithm is only one part of the overall solution. The integration of results or scores into the clinical workflow must be carefully considered in collaboration with all stakeholders to ensure that the AI‑enabled application provides meaningful information at the right time to support decisions that are beneficial to patients.
Additionally, most institutions have not invested in a general predictive analytics infrastructure that both captures live data in a scalable and secure fashion and enables the parallel deployment of algorithms in a real‑time environment. Without this enabling technology, researchers face a significant barrier in accessing potentially siloed data from a multiplicity of sources, running their predictive models at scale and distributing results to the bedside.
Together, these challenges constitute the “last mile” problem and should ideally be addressed up front as part of the overall solution.
MHN: What do you hope attendees walk away with after your discussion?
Spaeder: We hope attendees walk away understanding that predictive analytics powered by machine learning can meaningfully improve patient outcomes by using real‑time bedside monitoring data to detect deterioration early and that these solutions can scale across time and institutions when built correctly.
Equally important, successful adoption requires more than just algorithms. It demands a dynamic, multidisciplinary clinical integration strategy and a strong digital health infrastructure foundation.
Dr. Michael Spaeder's session “When Risk Becomes Visible: How Predictive Models Can Impact Care” is scheduled for Tuesday, March 10th, from 3:30 p.m. – 4:30 p.m. in Palazzo M I Level 5 at HIMSS26 in Las Vegas.
0
Comments
Want to join the conversation?
Loading comments...