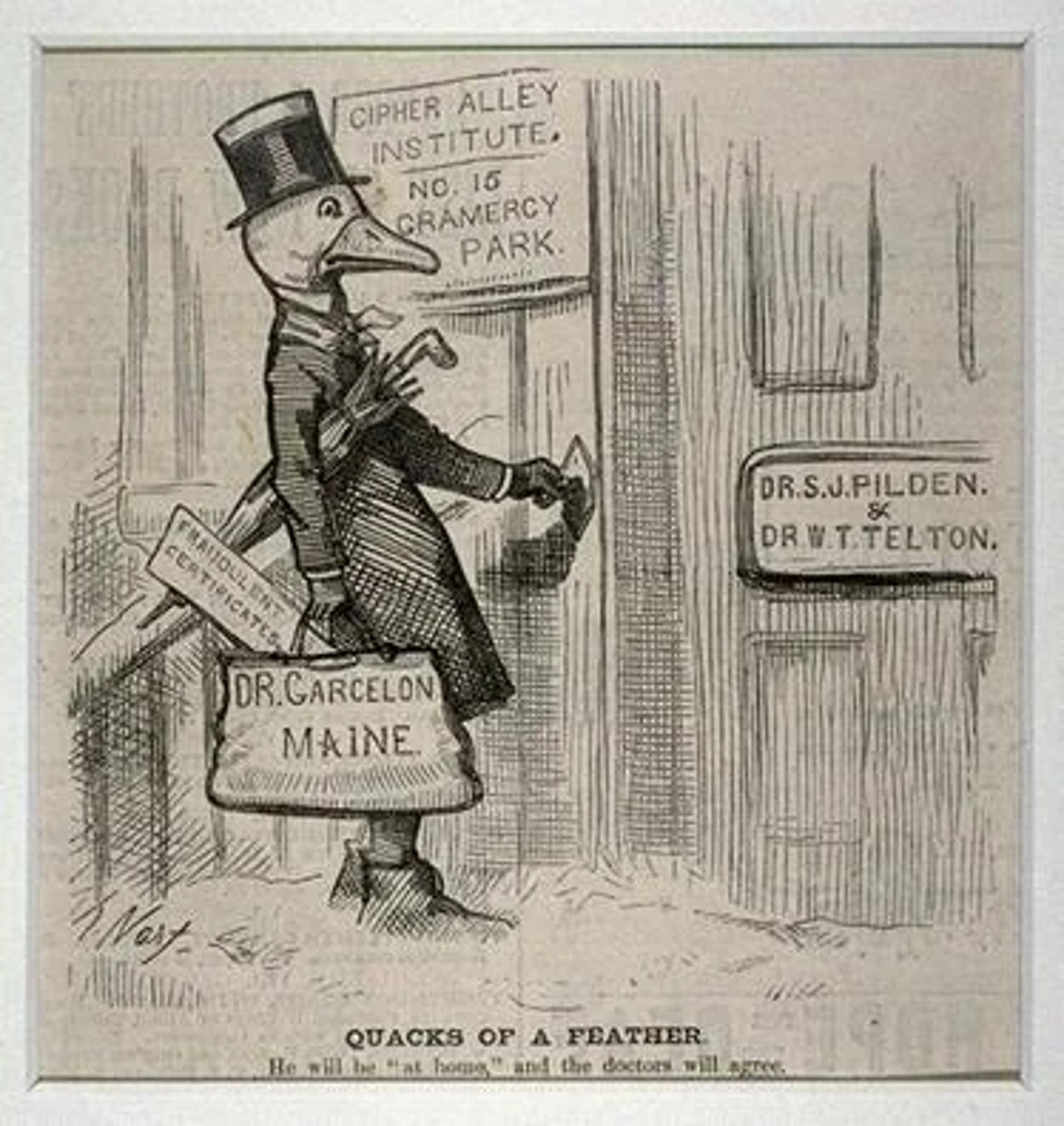
The FDA: Promoting Quack Nostrums Based on “Incredible Stories” While Rejecting Vaccines Despite Successful RCTs
•February 13, 2026
0
Why It Matters
Regulatory uncertainty inflates development costs, delays market entry, and may deter investment in next‑generation vaccines, reshaping the biotech competitive landscape.
Key Takeaways
- •FDA rejected Moderna's mRNA flu vaccine despite phase‑3 success
- •Trial showed 27% better efficacy than standard Fluarix
- •Regulatory shift raises costs and delays for vaccine developers
- •Industry warns of defensive strategies due to unclear guidance
- •Alternative flu vaccine grants favor traditional approaches over mRNA
Pulse Analysis
The FDA’s refusal to file Moderna’s mRNA flu vaccine underscores a growing disconnect between regulatory expectations and the data emerging from large‑scale clinical trials. While the company completed two phase‑3 studies with over 43,800 participants and a $750 million investment, the agency argued that the comparator—Fluarix—did not represent the optimal U.S. standard of care. This rationale appears at odds with prior FDA advice and with approvals granted by health authorities in Canada, the EU and Australia, raising questions about the consistency of the agency’s evidentiary standards for novel platforms.
For biotech firms, shifting regulatory goalposts translate directly into higher cash burn and longer timelines. Companies now must allocate additional resources to redesign trials, secure alternative comparators, or engage in prolonged negotiations, all of which erode the financial incentives that originally drove rapid mRNA development. The broader industry response points to a defensive posture: firms may favor established vaccine technologies over innovative candidates to avoid regulatory surprises, potentially stalling the pipeline of next‑generation products that could address seasonal flu more effectively.
Investor sentiment reflects this uncertainty, with market participants warning that the FDA’s stance could dampen enthusiasm for mRNA flu candidates and shift capital toward traditional vaccine manufacturers. As large grants continue to favor conventional approaches, the competitive advantage of mRNA platforms may diminish unless clear, predictable pathways are re‑established. Stakeholders across the biotech ecosystem are calling for transparent, stable guidelines that balance rigorous safety oversight with the agility needed to bring transformative vaccines to patients promptly.
The FDA: Promoting Quack Nostrums Based on “Incredible Stories” While Rejecting Vaccines Despite Successful RCTs
“In drug development, lack of regulatory clarity and consistency can be more damaging than regulation itself.”
As wise SBM readers already know, Dr. Vinay Prasad unilaterally overruled apolitical FDA experts, personally deciding the agency would not even review Moderna’s mRNA flu vaccine even though Canada, Australia, and the EU (including Denmark) agreed to do so. The vaccine, which can be updated more rapidly than traditional flu vaccines, was studied in two phase‑3 studies that enrolled over 43,800 participants at a cost of $750 million. It was 27 % more effective at preventing symptomatic flu and 49 % more effective against hospitalization than Fluarix, the comparator vaccine and ostensible source of controversy.
According to an article about Dr. Prasad’s edict by STAT:
In the “refusal‑to‑file” letter, Prasad wrote that the FDA does not consider the study in the application to be “adequate and well‑controlled” — the standard for FDA approval under the law — because “your control arm does not reflect the best‑available standard of care in the United States at the time of the study.” He added: “I note that this determination is consistent with FDA’s advice given to you prior to your study.”
In its press release, Moderna acknowledged that the FDA told the company the agency would prefer it use a different vaccine — one with a higher dose of influenza antigen targeted at older people, for whom the higher‑dose vaccines are recommended. But the company reproduced language from the FDA showing the agency had prefaced this request with: “while we agree it would be acceptable to use a licensed standard dose influenza vaccine as the comparator in your Phase 3 study.”
Notably, a recent RCT of 332,438 participants found that “a high‑dose inactivated influenza vaccine did not result in a significantly lower incidence of hospitalization for influenza or pneumonia than a standard dose among older adults.” Additionally, Moderna ran an immunogenicity trial of people older than 65 comparing their mRNA vaccine against a high‑dose egg‑based comparator. The mRNA vaccine was safe and resulted in superior inhibition titers.
The STAT article continued:
Stephen Hoge, Moderna’s president, told STAT in an interview that the company decided to compare its vaccine to Fluarix, a licensed vaccine made in chicken eggs by GSK, because that was the licensure path followed by other influenza vaccine‑makers. He also pointed out that Moderna wanted to compare its vaccine to a single comparator across the 50‑and‑up age group, and said that using the high‑dose vaccine might have complicated obtaining regulatory clearance in other countries.
The FDA “had previously indicated that it would be acceptable and it was exactly the same approach everyone has used,” Hoge said, adding that the company is “pretty surprised, pretty confused and want to seek an understanding of why has this changed so dramatically from a recommendation to we won’t even review the file.”
“Vaccines are radioactive now”
There is no question that Kennedy, who already decimated funding for mRNA vaccines, will be delighted with Dr. Prasad’s decree, as will top NIH officials Drs. Matthew Memoli and Jeffery Taubenberger, who were recently awarded a non‑reviewed $500 million grant to develop a flu vaccine using an inactive virus.
In contrast, who in their right mind would volunteer for a vaccine RCT today? What company would even bother trying? As Dr. Ruxandra Teslo wrote in her article “The FDA Should Not Change Its Mind Last Minute”:
I often say that in drug development, lack of regulatory clarity and consistency can be more damaging than regulation itself. Clear rules, even when stringent, can be understood and navigated. But unclear or constantly shifting expectations can be much harder to efficiently deal with.
That uncertainty doesn’t just slow individual programs, but also reshapes behavior across the biotech ecosystem in a negative way. Lack of regulatory clarity fosters a culture of defensive decision‑making, where companies avoid innovative clinical development strategies and default to more conservative, expensive paths simply because they lack confidence in how the FDA might respond. Over time, this dynamic drives up trial costs, prolongs timelines, and ultimately reduces the number of truly innovative therapies that reach patients.
Indeed, even before this latest debacle, Moderna’s CEO said he was cutting back on vaccine trials, and responding to the latest news former Gavi CEO Seth Berkley said:
This is going to change the dynamic, not just for Moderna, but for other vaccine companies. If you’re a manufacturer, now you’re saying, “do we know what the rules are?” Because they changed the goalposts here after a very, very large clinical trial, to all of a sudden say they’re not going to even look at it.
“Vaccines are radioactive now,” said one biotech investor. Despite their professed love of data and evidence, this is what the EBM gurus and “medical conservatives” have delivered to us in the real world.
“Incredible stories from doctors who have seen dramatic improvement”
While this is all bad enough, it’s worthwhile to remember how the FDA approached Kennedy’s pet autism “cures.” Listen as Dr. Makary says anecdotes alone are sufficient.
Shortly after that interview, the headlines read “Largest Leucovorin‑Autism Trial Retracted.”
This is our FDA today. Quack nostrums get approved based on “incredible stories,” while vaccines get dismissed out of hand despite multiple successful RCTs. Our FDA leaders call this “gold‑standard science, transparency and common sense.” At least they are not fooling anyone anymore. Everyone knows it’s anti‑vaxx politics all the way down.
Author: Dr. Jonathan Howard – neurologist and psychiatrist, author of We Want Them Infected: How the failed quest for herd immunity led doctors to embrace the anti‑vaccine movement and blinded Americans to the threat of COVID.
0
Comments
Want to join the conversation?
Loading comments...