AI-Based Platform Supports Community Health Workers in Street Medicine Program
•February 20, 2026
0
Why It Matters
The solution demonstrates a scalable, financially sustainable way to deliver whole‑person care to homeless populations, addressing a critical gap in value‑based health systems and informing CalAIM policy implementation.
Key Takeaways
- •AI prompts CHWs, auto‑generates clinical records
- •Reduces CalAIM documentation burden for providers
- •Enables 2.5‑3× patient capacity per clinician
- •First‑day provider contact reaches 65% of enrollees
- •Expansion targets 10,000 Bay Area patients
Pulse Analysis
Street‑medicine programs have long struggled with fragmented data, heavy paperwork, and limited clinician bandwidth, especially under California’s ambitious CalAIM whole‑person care model. By embedding AI into tablets carried by community health workers, Akido transforms each encounter into a structured, searchable record that feeds directly into physicians’ electronic health records. This technology not only streamlines compliance with complex reimbursement requirements but also empowers workers with lived experience to capture nuanced social determinants, bridging the gap between outreach and clinical decision‑making.
The early results are striking: 65% of newly enrolled patients connect with a provider on the first day, average visit frequency climbs to 2.2 per month (with high‑acuity patients receiving 4‑5 visits), and prescription turnaround for critical medications drops to 24 hours. Providers report a 2.5‑to‑3‑fold increase in the number of patients they can manage, while retention stays above 67%. By automating documentation, the platform lifts the administrative load that previously limited provider scalability, allowing clinicians to focus on direct care rather than paperwork.
Beyond immediate outcomes, the Akido model offers a template for other jurisdictions seeking to meet CalAIM goals without sacrificing financial viability. Its data‑rich approach creates a robust evidence base that can be shared with legislators and payers, accelerating policy adoption of technology‑enabled, whole‑person care. As the program scales to the Bay Area, it could serve as a national benchmark for integrating AI, community health workers, and value‑based reimbursement structures to improve health equity for the nation’s most vulnerable populations.
AI-Based Platform Supports Community Health Workers in Street Medicine Program
By David Raths · Feb. 20, 2026
Key Highlights
-
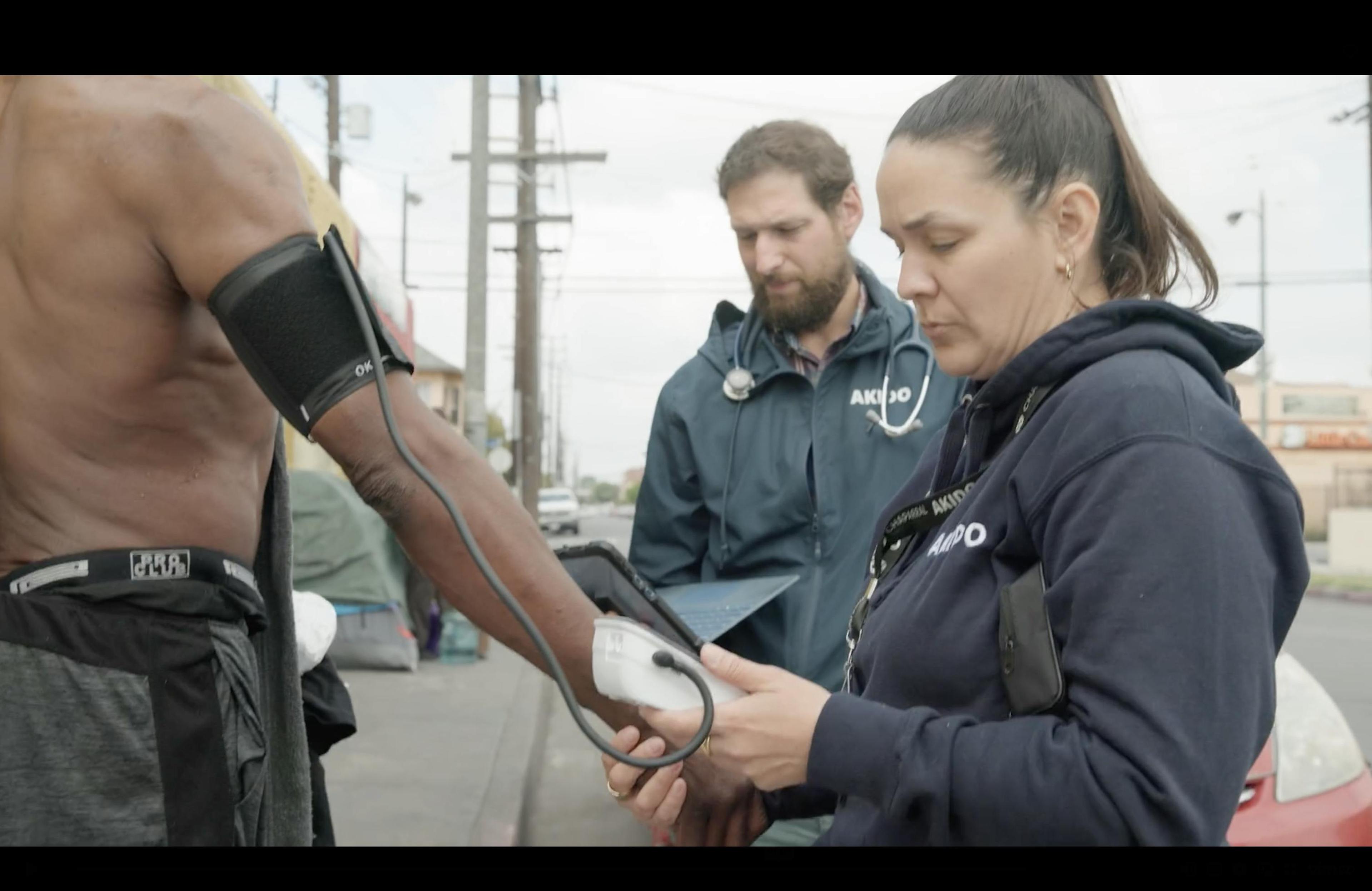
In this new model, Akido's platform supports community health workers with real‑time data collection, documentation, and patient‑engagement tools.
-
The program aims to address complex social needs such as housing and food access, aligning with CalAIM's whole‑person care model.
Courtesy of Akido Labs
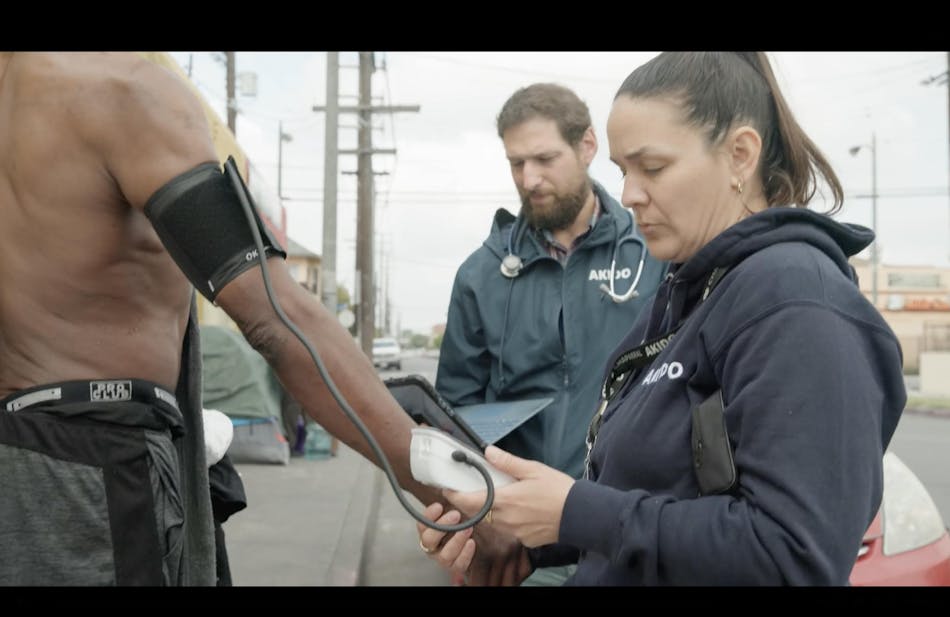
Several California‑based organizations are coming together to use AI technology and community health workers to bolster street‑medicine programs. An initiative started in Southern California using Akido Labs’ tech‑supported care model will launch in the Bay Area in March. Several stakeholders spoke with Healthcare Innovation about the potential impact.
The nonprofit Future Communities Institute (FCI) will serve as the convener of the group, working with the provider network Akido Labs as well as community‑based organizations Five Keys and ReImagine Freedom. Five Keys focuses on people experiencing homelessness, with about 25,000 people in their network. ReImagine Freedom serves formerly incarcerated women. As the convener, FCI is co‑designing an evaluation framework that prioritizes the expressed needs of each community and provides consistent data reporting across partners.
“Whole‑person care is a promise that we can serve all of the above in a single model,” said Emma Mayerson, co‑founder and executive director of Future Communities Institute. “The issue has been that there are very few models that are leveraging CalAIM that have achieved financial sustainability and achieved scale. There's a huge administrative burden associated with CalAIM reimbursements and it's a very complex model to implement. What FCI is really excited about is CalAIM’s promise being met with an innovative company like Akido, which is bringing AI into the picture to be able to make it financially sustainable and scalable without sacrificing quality.”
Akido describes itself as an AI‑native healthcare provider network. It has 500,000 patients across the country, 240 providers, 100‑plus clinics, and 25 specialties. The company also has a major street‑medicine presence in California. It is using AI from the ground up in how it delivers care, to expand access to patients who struggled to get care in the traditional healthcare system.
Akido also can shift a lot of the reporting and documentation burden of CalAIM off of the street‑medicine providers, who are overstretched. The harmonization of records and the tracking of their ongoing engagement is critical, the partners say.
Matt Siegler, Akido’s chief network officer (formerly of Kaiser Permanente and NYC Health & Hospitals), explained:
“Street‑medicine providers are a special breed. It’s difficult to find people who are committed enough to do this work, and it's difficult to sustain the work. You have to enable people and support them with a broad team of caregivers. You have to provide them with ways to reach these patients and follow up on their needs in an ongoing way. Doing that with paper and pen and physically out in the street every day as an M.D., going from tent to tent or shelter to shelter, can be very challenging and is not sustainable from a financial perspective for most providers.”
Akido’s model involves enabling community health workers and others with lived experience and cultural competency to reach people. The information they gather is sent to the physician’s device for review; physicians can then order through the EHR and decide the next step in the patient’s journey. Siegler calls this the “secret sauce”:
“Lots of people have technology, but they don't want to deploy it for this population.”
How AI Is Used
Siegler said the AI runs on a tablet or laptop that a community health worker or care manager carries during a patient visit. It prompts them with questions and completes a record for the physician to review, enabling a more informed conversation. The AI also powers Akido’s electronic health record and longitudinal tracking of individuals’ needs.
“I think the transformative piece is really that the community health worker can collect a lot of the information that's needed,” he said.
The model is already active in Los Angeles and Kern County, and the partners are building capacity for up to 10,000 patients in the Bay Area.
Early Results
-
65 % of patients see a provider on the first day of enrollment.
-
Patients average 2.2 visits per month (high‑acuity patients 4–5 visits/month), far exceeding typical primary‑care access.
-
Retention rate is over 67 %.
-
Prescription turnaround for critical, life‑saving medicines (e.g., opioid‑abuse‑reduction prescriptions) is about 24 hours.
-
Providers are seeing 2.5–3 × the number of patients they could before the technology was deployed.
Looking Ahead
Mayerson noted that FCI is interested because the model could help the state improve CalAIM:
“We have to be documenting and amplifying the examples that do exist of being able to effectively achieve the promise of CalAIM. The use of technology to create that force multiplier is a key component, and we need to be embracing its potential and its impact… We are making sure that we are coming to legislators, locally, statewide and nationally, to share what we're seeing and to advocate for the proliferation of what works.”
About the Author
David Raths is a Contributing Senior Editor for Healthcare Innovation, focusing on clinical informatics, learning health systems and value‑based care transformation. He has been interviewing health‑system CIOs and CMIOs since 2006.
0
Comments
Want to join the conversation?
Loading comments...