CCTA Becoming an Essential Tool for Interventional Cardiologists
•February 13, 2026
0
Why It Matters
By offering a cheaper, high‑resolution alternative that combines anatomy and physiology, CCTA expands access to optimal PCI planning and cuts unnecessary invasive procedures, reshaping cardiac care economics and outcomes.
Key Takeaways
- •CCTA enables pre‑procedure PCI planning
- •Photon‑counting CT improves plaque visualization, reduces indeterminate cases
- •FFR‑CT combines anatomy and physiology, replacing nuclear gatekeeper
- •Lower cost than intravascular imaging expands global access
- •Early CCTA use cuts unnecessary invasive angiographies
Pulse Analysis
Coronary computed tomography angiography (CCTA) is rapidly moving from a diagnostic adjunct to a central component of interventional cardiology workflows. By delivering high‑resolution anatomical maps before patients enter the cath lab, CCTA allows physicians to outline stent sizing, lesion crossing strategies, and even anticipate complications. The integration of fractional flow reserve derived from CT (FFR‑CT) adds functional assessment, effectively merging the physiological gatekeeping traditionally performed by nuclear scans with an anatomical study. This dual capability reduces reliance on costly intravascular imaging and streamlines decision‑making for intermediate‑risk patients.
Photon‑counting detector CT represents the next leap in coronary imaging, capturing individual photons to produce ultra‑high‑resolution scans that resolve soft‑plaque composition and penetrate stent struts. St. Francis’s dedicated cardiac photon‑counting units have already demonstrated a measurable drop in indeterminate CCTA cases referred for invasive angiography, according to a recent JACC publication. Patients who do proceed to the cath lab are more likely to receive percutaneous coronary intervention, indicating that the technology not only refines diagnosis but also improves procedural efficiency and resource utilization across cardiac centers. Moreover, photon‑counting systems operate at lower radiation doses while delivering raw data that can be reconstructed with advanced AI‑driven algorithms, further accelerating turnaround times for clinicians.
The convergence of affordable CCTA, FFR‑CT, and photon‑counting technology is poised to democratize PCI planning, especially in regions where intravascular imaging remains prohibitively expensive. Hospitals that adopt a CT‑first strategy can expect shorter hospital stays, fewer unnecessary catheterizations, and a clearer revenue stream from high‑throughput imaging suites. However, widespread implementation hinges on training interventionalists in CT‑based workflow, integrating sophisticated software platforms, and securing reimbursement policies that recognize the cost‑savings of upstream diagnostics. As guideline committees begin to cite emerging evidence, CT‑guided PCI is likely to become the new standard of care.
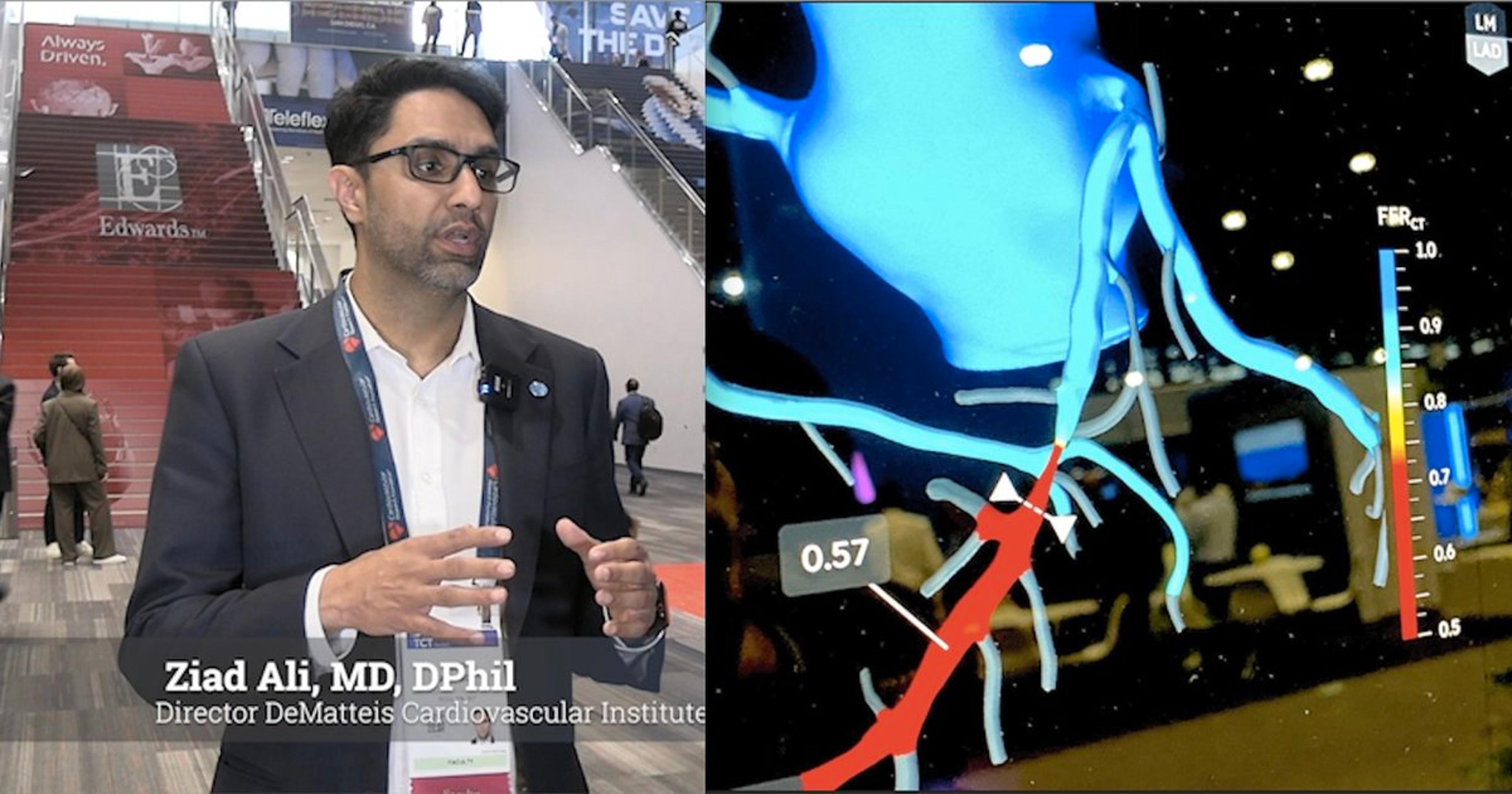
CCTA becoming an essential tool for interventional cardiologists
Dave Fornell · February 13, 2026 · Cardiovascular Business
“It really allows all of the PCI planning to be done upfront before you even walk into the cath lab,” Ali explained.
This approach may also address persistent gaps in the use of intravascular imaging. While adoption of optical coherence tomography (OCT) and intravascular ultrasound (IVUS) has increased significantly over the past decade, utilization remains far from universal, even with its inclusion in modern guidelines. He noted that the cost of intravascular imaging and FFR catheters remains a barrier, and CT offers a more accessible alternative.
“CT is a very cheap, highly effective anatomical assessment of coronary disease,” Ali said.
He believes CT can help “democratize” access to algorithmic PCI planning strategies worldwide. In addition, FFR‑CT strengthens CCTA’s role as a gatekeeper.
“It’s hard to bring a patient to the cath lab without an assessment of ischemia,” Ali said. “FFR‑CT allows you to do that upfront.”
While nuclear imaging, which provides only physiologic data, has long been that gatekeeper, he said CT delivers both anatomy and physiology in a single test.
Ali’s hospital has a very low threshold for using CCTA with FFR‑CT, particularly in intermediate‑risk patients whose symptoms might be managed medically.
Photon‑counting CT enhances coronary imaging
The addition of photon‑counting CT has further refined CCTA with even clearer imaging of soft plaques and the ability to see through stents and classified lesions. St. Francis now has two of these scanners dedicated to cardiac imaging. The technology enables higher‑resolution imaging by detecting individual photons rather than accumulating energy signals.
Ali’s team recently published findings in JACC showing that photon‑counting CT significantly reduced indeterminate cases sent to the cath lab.[1] Patients who did proceed to invasive angiography were far more likely to undergo PCI, reducing unnecessary procedures and resource use.
“I think the future of interventional cardiology is photon‑counting CT along with CT‑guided PCI,” Ali said.
For centers still relying on workflows established more than a decade ago and not using routine cardiac CT, Ali said they really should consider the benefits of moving to a CCTA workflow.
“CT‑guided PCI provides you anatomy and physiology. It’s a readily available tool you can get all of the things that you need to do with intravascular imaging, pre‑PCI. It’s just a question of using the right software and tools to help you become familiar with it. Once you learn it, it becomes the standard of care.”
Reference
- Koshiro Sakai, Doosup Shin, Mandeep Singh, et al. Diagnostic Performance and Clinical Impact of Photon‑Counting Detector Computed Tomography in Coronary Artery Disease. JACC. Oct 27, 2024. Vol 85 No 4. DOI: 10.1016/j.jacc.2024.10.069.
About the author
Dave Fornell is a digital editor with Cardiovascular Business and Radiology Business magazines. He has been covering healthcare for more than 16 years, focusing on cardiology and radiology. Fornell is a five‑time winner of the Jesse H. Neal Award, the most prestigious editorial honor in specialized journalism. He produces more than 100 editorial videos each year, most of them interviews with key opinion leaders in medicine. Email: [email protected].
0
Comments
Want to join the conversation?
Loading comments...